
TRILLIANT
RETROSPECTIVE REVIEW: OPEN REDUCTION AND INTERNAL FIXATION OF ANKLE FRACTURES USING TRILLIANT GRIDLOCK ANKLE PLATING SYSTEM
Presented byBrett D. Sachs, DPM, FACFAS and Andrew Yang, DPMGRIDLOCK ANKLE PLATING SYSTEM
Introduction
Ankle fractures are a common injury to the lower extremities. Displaced fractures involving the ankle joint can be challenging injuries for a foot and ankle surgeon. The anatomic reduction of displaced ankle fractures has been shown to be a fundamental factor in providing stability to the ankle joint. In 1976, Ramsey and Hamilton showed that 1 mm of lateral talar shift will result in 42% loss of tibiotalar contact.1 For several years, the importance of anatomic reduction of displaced ankle fractures continued to be studied and compared to non-operative treatment. Operative treatment has consistently been shown to have superior clinical outcomes when compared to non-operative treatment of ankle fractures.2-4 In general, open reduction with internal fixation (ORIF) of displaced ankle fractures is currently considered the standard treatment.Throughout history, there has been an evolution of different surgical ORIF techniques involving the treatment of ankle fractures. These include tension banding, lag screws, 1/3 tubular plate, posterior anti-glide plate, lateral locking plate, fibula-pro-tibia technique, intramedullary nails, and minimally invasive percutaneous plating (MIPO). Each of these techniques has its advantages and disadvantages, but ultimately, they all aim to provide and maintain anatomic reduction of the fracture with stable fixation. The purpose of this study was to demonstrate the clinical and radiographic outcomes of using the Trilliant Surgical Gridlock Ankle Plating System in the surgical fixation of ankle fractures. (Figure 1)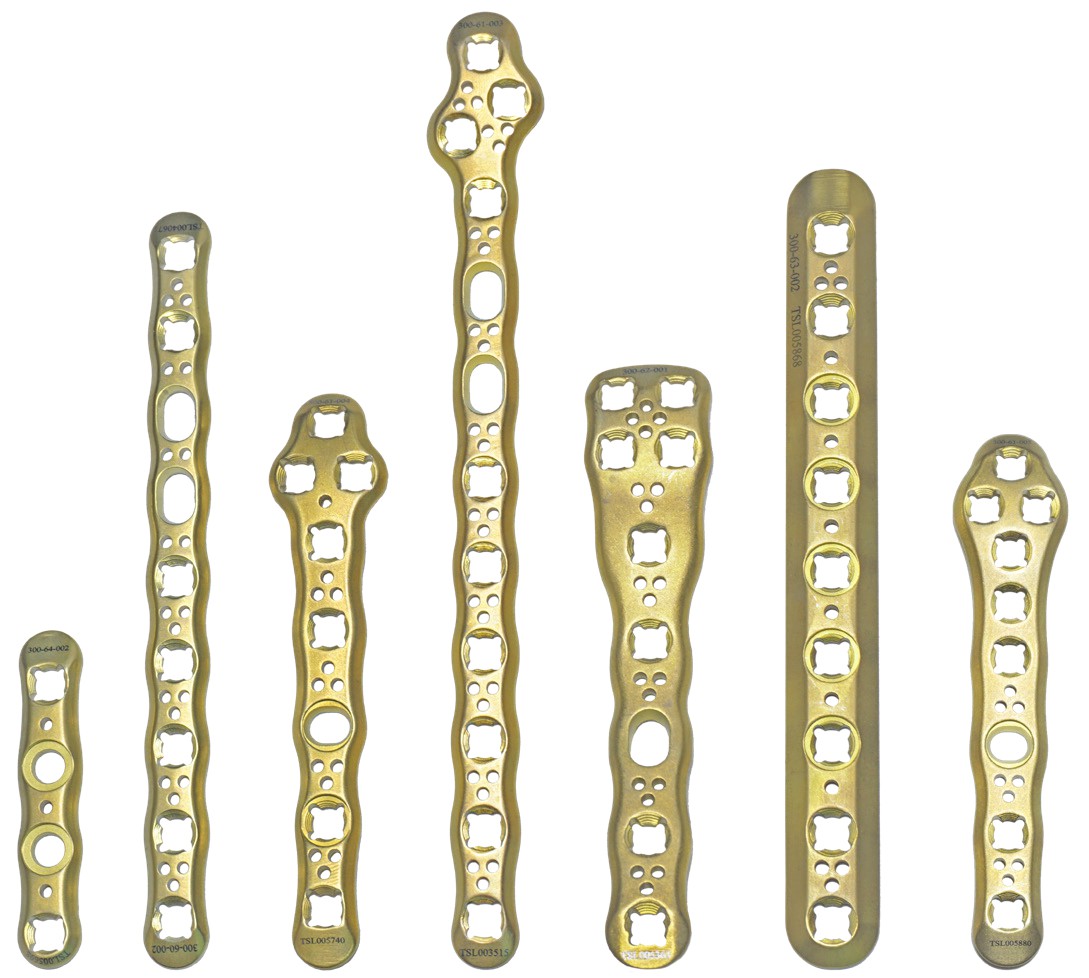 Figure 1. Gridlock Ankle Plating System (From left: Buttress Plate, VL Fibula Plate, VL Distal Fibula Plate, Right/Left Contoured VL Fibula Plate, VL Tibia Plate, 1/3 Tubular Plate, Universal Contoured VL Fibula Plate)
Figure 1. Gridlock Ankle Plating System (From left: Buttress Plate, VL Fibula Plate, VL Distal Fibula Plate, Right/Left Contoured VL Fibula Plate, VL Tibia Plate, 1/3 Tubular Plate, Universal Contoured VL Fibula Plate)
Patients and Methods
We conducted a retrospective case series review of 10 patients who underwent surgical repair for various distal tibial and fibular ankle fractures from May 2016 to December 2017. Patients were not excluded based on coexisting comorbidities including diabetes mellitus, peripheral neuropathy, smoking, osteoporosis, or obesity. However, open fractures, pilon fractures, and patients involved in polytrauma were not included in this study. This study included 2 males and 8 females. The age range was 34-78 years with a mean age of 46 years. The time from injury to surgery ranged from 8-18 days with a mean time of 11.6 days. Five patients had diabetes mellitus type II. (Table 1)
| Age(years) | Sex | Past Medical History | Time from Injury toORIF (days) | Fracture Type | SyndesmoticScrew | Outcome |
| 53 | F | Hep. C, hypothyroidism, HLD | 13 | Weber B | No | Union |
| 29 | M | Asthma, Cancer, DM2 | 7 | Weber B | No | Union |
| 53 | F | None | 18 | Weber C | Yes | Union |
| 34 | M | Testicular Cancer, DM2, bipolar | 12 | Medial Malleolar | No | Union |
| 50 | F | HTN, GERD | 10 | Trimalleolar | No | Union, OCD |
| 78 | F | HTN, DM2, Cancer | 10 | Syndesmotic Disruption | Yes | Union |
| 61 | F | HTN, DM2, Cancer | 14 | Bimalleolar | No | Union |
| 42 | F | Anemia, Arthritis | 10 | Weber B | Yes | Union |
| 57 | F | HTN, HLD | 14 | Weber C | No | Union |
| 53 | F | HTN, DM2 | 8 | Bimalleolar | No | Union, OCD |
Table 1. Patient demographics
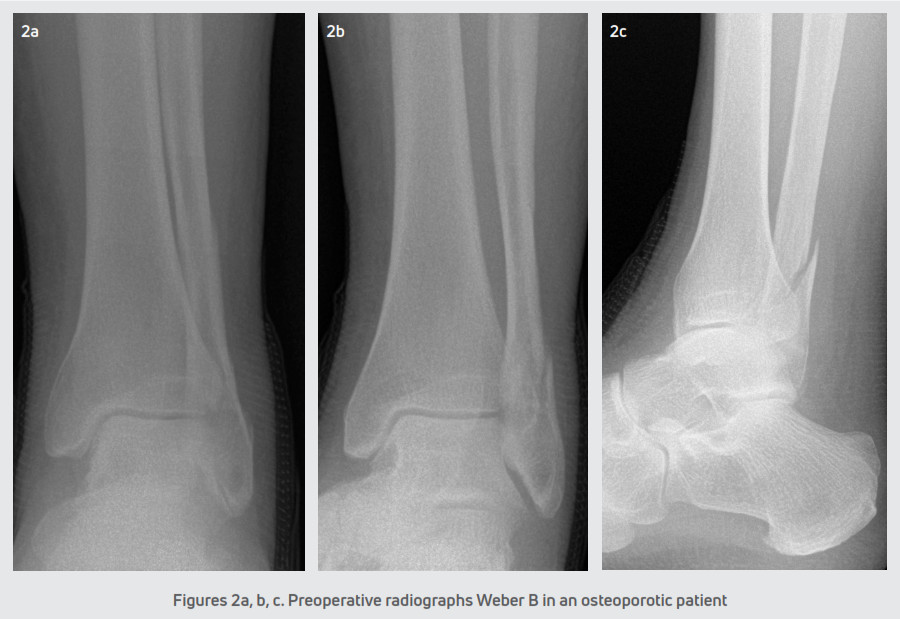
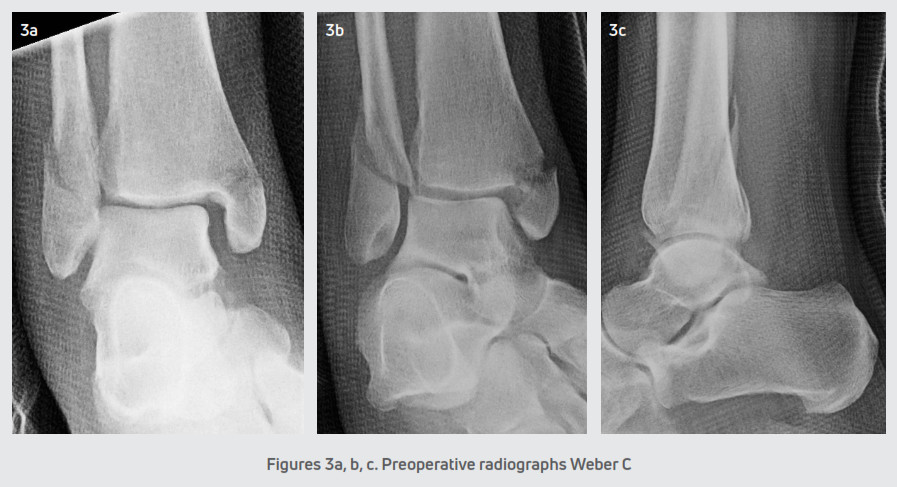
All the patients were seen at the senior author’s private practice for an evaluation. Patients were splinted and initially kept non-weight bearing until the scheduled date for surgery. Open reduction and internal fixation of the ankle fractures were performed within 1 and 2.5 weeks post-injury depending on the edema and condition of the soft tissue envelope at the initial presentation. Each patient received preoperative radiographs. (Figures 2 and 3) Also, additional radiographs were taken at postoperative visits typically at weeks 4, 8, and 12. During each postoperative appointment, the fracture sites were examined for clinical signs of healing.
 Procedure
Procedure
All patients were positioned supine and administered general anesthesia. In addition, patients received a popliteal block and a thigh tourniquet was utilized for hemostasis. For all fibular fractures, a direct lateral approach was performed with a linear longitudinal incision centered over the distal fibula. The fracture hematoma was evacuated and the fracture fragments were reduced with fracture reduction clamps. A solid core 3.5 mm Trilliant Gridlock ankle plating screw was placed across the fracture site utilizing standard AO principles and techniques. Then, a Trilliant Gridlock Ankle Contoured VL Fibula Plate was placed over the lateral fibula and fixated with a combination of locking and non-locking screws. The Trilliant variable angle guide was typically used in the distal fibula and screws had unicortical purchase in order to avoid violation of the tibiotalar joint. In the proximal fibula, the Trilliant static locking drill guide was used and bicortical purchase of the screw was achieved. If a medial malleolar fracture was present, then a linear longitudinal incision was made overlying the medial malleolus. The fracture hematoma was evacuated, and the fracture was manually reduced. Then, either two 4.0 mm Trilliant Tiger cannulated bone screws or a medial tibial Trilliant Gridlock ankle plate was utilized for fixation. The medial tibial Trilliant Gridlock ankle plate was placed over the medial aspect of the tibia and fixated with locking and non-locking screws. The ankle syndesmosis was stressed under fluoroscopy in all cases utilizing the Cotton hook test and/or the external rotation test. If disruption of the ankle syndesmosis was identified, a large bone clamp was used for reduction. Next, two Trilliant tapered core syndesmotic screws were placed through the ankle plate in a lateral to a medial direction crossing four cortices in order to stabilize the syndesmosis. The syndesmotic screws were typically removed approximately 8-10 weeks following the index procedure and replaced with suture button flexible fixation to maintain syndesmotic stability. Intraoperative fluoroscopy was used to confirm the anatomic reduction of the fracture and proper hardware placement. The one patient with a posterior malleolus fracture did not require internal fixation.
The incisions were closed in a standard layered fashion and a sterile, compressive dressing was applied. All patients were immobilized with a posterior splint and were initially non-weight bearing. Patients were seen for the first postoperative visit within 5-6 days for a wound evaluation. A sterile dressing and posterior splint were reapplied and patients returned at two weeks for suture removal. The postoperative course consisted of non-weight bearing in a posterior splint for 2-3 weeks. In ankle fractures with a stable syndesmosis (Figure 4), patients were transitioned into a CAM boot at 3 weeks and began protected partial weight-bearing with physical therapy. After 6 weeks, patients were transitioned to a supportive athletic shoe with an ankle brace and the final follow-up was at 12 weeks. In ankle fractures that required syndesmotic repair (Figure 5), patients were transitioned into a CAM boot and began protected partial weight-bearing at approximately 8-10 weeks. Patients were progressed into normal shoe gear at 12 weeks and aggressive physical therapy. Patients were discharged at 4-6 months and followed up as needed.
 Results
Results
In the series of 10 patients, all patients showed clinical and radiographic evidence of healing at the fracture site. Radiographs were obtained at approximately 8-10 weeks postoperative revealing 100% union at the fracture sites. There were 3 patients who continued to have postoperative pain 6 months after surgery. Two patients had osteochondral lesions of the talus identified at the initial surgery. These 2 patients subsequently underwent ankle arthroscopy and microfracture of the osteochondral lesion. Despite anatomic reduction, the third patient showed early signs of posttraumatic arthritis of the tibiotalar joint. There were no complications related to wound healing, infection, or painful hardware. There were no non-unions, malunions, or revision surgery.
Discussion
The origin of locking plate technology can be traced to a monocortical fixator by Carl Hansmann in 18865 and was further developed by Paul Reinhold in 19315. Reinhold developed the initial form of locking plates by patenting the thread in thread fixation of screws to plates. There were multiple screw fixation systems developed in the late 1900s including the Litos system in 19746 and Zespol in 19827, which began to popularize the concept of locking plates and screws. In 1995, the Arbeitsgemeinschaft für Osteosynthesefragen, Association for the Study of Internal Fixation (AO), developed another locking system called point contact fixator (PC-fix).8 The Less Invasive Stabilization system was introduced in 20019 followed by the locking compression plate (LCP).10
Trilliant Surgical developed the Gridlock Ankle Plating System, which contains all of the current advancements in locking plate technology and design. The plates are low profile, pre-bent, and pre-contoured with vanishing edges. There is a built-in skive on the proximal and distal edges to assist in plate placement. The plates have unique triple relief holes intended for increased plate malleability for any necessary plate contouring without compromising the functional aspects of the plate. On the underside of the plate, there is a unique crosshatch design that incorporates the principles of a limited contact plate. The principles of a limited contact plate have been theorized, in published literature, to decrease stress shielding and minimize vascular damage to the bone.8 In addition, the ankle plates have polyaxial locking ability that are used in combination with low-profile locking and non-locking screws. The syndesmotic screws have a tapered core design for greater strength.
Kim et al. performed a biomechanical cadaveric study comparing locking versus conventional plates for the fixation of fibular fractures.11 The study revealed that locking plates had equivalent fixation across different bone marrow densities and the failure to load of locking plates were independent of bone marrow density. Locking plates were not only shown to be mechanically equivalent to a lag screw and 1/3 tubular plate construct, but also have an advantage in osteoporotic bone. Another study by Moriarty et al. compared the complication rates between locking and nonlocking plates in distal fibular fractures in 160 patients over 2 years.12 The authors reported that the complication rate of the locking plate was similar to the non-locking plate, 13.5% vs. 15.4% respectively. A biomechanical study by Wilkens et al. compared uniaxial and polyaxial locking plates in distal femur fractures.13 The study showed that polyaxial locking plates had superior mean axial stiffness, mean torsional stiffness, and mean ultimate load to failure compared to uniaxial locking plates. Polyaxial locking plates also had a significantly less mean irreversible deformation caused by cyclic axial loading.13
In conclusion, our case series of 10 patients showed that using the Trilliant Surgical Gridlock Ankle Plating System for ankle fractures allowed for adequate anatomic reduction, stable internal fixation, and fracture healing. All patients had successful union and no clinical pain at the site of fracture. There were 3 patients that continued to have pain 6 months postoperative that were related to the inherent mechanism of injury. In these 10 patients, the use of the Trilliant Surgical Gridlock Ankle Plating System produced a stable internal construct to promote fracture healing and provide a reasonable option for the treatment of ankle fractures.
References
- Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg. 1976;58(3):356357.
- Phillips WA, Schwartz HS, Keller CS, Woodward HR, Rudd WS, Spiegel PG, Laros GS. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg. 1985;67(1):67-78.
- Ali MS, McLaren CA, Rouholamin E, O’Connor BT. Ankle fractures in the elderly: nonoperative or operative treatment. J Orthop Trauma. 1987;1(4):275-280.
- Makwana NK, Bhowal B, Harper WM, Hui AW. Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age: a prospective, randomized study. Bone Joint J. 2001;83(4):525-529.
- Cronier P, Pietu G, Dujardin C, Bigorre N, Ducellier F, Gerard R. The concept of locking plates. Orthop Traumatol Surg Res. 2010;96(4):S17-S36.
- Russell TA. A historical perspective of the development of plate and screw fixation and minimally invasive fracture surgery with a unified biological approach. Tech Orthop 2007;22:186-90.
- Ramotowski W, Granowski R. Zespol, an original method of stable osteosynthesis. Clin Orthop Relat Res 1991;272:67-75.
- Auer J, Bishop SJ, Bresina SJ, Buchanan JS, Furst T, Gautier E, Iselin U, Kaegi B, Lischer C, Matter G, Matter P, Montavon PM, Munch TWH, Perren SM, Rahn BA, Savoldelli D, Schatzker J, Tepic S, van Frank Haasnoot E. Point contact fixator part I. Scientific background, design and application. Injury. 1995;26(2):B1-B50.
- Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur less invasive stabilization system. Injury. 2001;32:SC24-31.
- Sommer C. Locking compression plate. Injury. 2003;34(2):1-76.
- Kim T, Ayturk UM, Haskell A, Miclau T, Puttlitz CM. Fixation of osteoporotic distal fibula fractures: a biomechanical comparison of locking versus conventional plates. J Foot Ankle Surg. 2007;46(1):2-6.
- Moriarty A, Ellanti P, Mohan K, Fhoghlu CN, Fenelon C, McKenna J. A comparison of complication rates between locking and non-locking plates in distal fibular fractures. Orthop Traumatol Surg Res. 2018;104(4):503-506.
- Wilkens KJ, Curtiss S, Lee MA. Polyaxial locking plate fixation in distal femur fractures: a biomechanical comparison. J Orthop Trauma. 2008;22(9):624-628.
T 800.495.2919F 877.778.3864727 North Shepherd Drive, Suite 100 I Houston, TX 77007 I U.S.A.djoglobal.comCopyright © 2021 by DJO, LLC900-30-007 Rev C
NOTE: The views and opinions expressed in this white paper are those of the authors. DJO, LLC is a manufacturer of orthopedic implants and does not practice medicine. Only an orthopedic, or foot and ankle surgeon can determine what treatment is appropriate. The contents of this document do not constitute medical, legal, or any other type of professional advice. This material is intended for the sole use and benefit of the DJO, LLC sales force and physicians. It is not to be redistributed, duplicated, or disclosed without the express written consent of DJO, LLC. For more information on risks, warnings, and possible adverse side effects refer to the Instructions for Use provided with the device.
References
[xyz-ips snippet=”download-snippet”]

 Procedure
Procedure Results
Results